Driver of neurodegenerative diseases revealed
Lysosomes, tiny compartments within cells known as the garbage disposals for molecules that need to be degraded, are critical to cell function and a person’s health; disruption of lysosomal protein function is linked to a variety of neurodegenerative diseases. Identifying how mutations in the genes coding for these proteins lead to disorders could provide scientists not only a better understanding of disease, but also a path to new treatments.
In a new study published on September 14 in Science, Monther Abu-Remaileh, assistant professor of chemical engineering and of genetics and Institute Scholar of Sarafan ChEM-H at Stanford University, identified the function of a lysosomal protein known to be dysregulated in a rare but fatal neurodegenerative disease. His team discovered that this protein drives a key step in the synthesis of a lipid molecule called bis(monoacylglycero)phosphate, or BMP, which is known to be critical in Alzheimer’s, Parkinson’s, and other neurodegenerative diseases. Uncovering this long-elusive protein not only gives scientists a handle to develop new drugs for those diseases, but also establishes a new paradigm in cell biology: the lysosome, long thought of as the center of molecule-breaking, is also home to molecule-making.
“Now that we know how the cell makes BMP, we can develop ways to activate it and hopefully find ways to counteract and improve age-related neurodegeneration,” said Abu-Remaileh.
Searching for 773
Abu-Remaileh is investigating a series of rare diseases linked to lysosomal dysfunction. In the cases of many of these so-called lysosomal storage disorders, scientists know that a particular genetic mutation leads to disease. That genetic information contains the instructions for making a protein that resides in the lysosome, but what that protein does in healthy individuals—and therefore why the mutation leads to sickness—has been unknown in many of these disorders.
The lead author of this study, biochemistry PhD student Uche Medoh, was working on two different projects that serendipitously merged. In one, he was studying a gene called CLN5, a risk factor for Alzheimer’s disease. CLN5 mutations are very rare, and patients suffer from infantile and juvenile neurodegeneration and premature death. Medoh was trying to figure out the function of the protein encoded by the CLN5 gene. At the same time, in a separate project, he had started looking into a lipid, a fatty molecule central to normal cell functions, called BMP. BMP is an important regulator of lysosomal function and is implicated in a variety of neurodegenerative diseases; BMP levels are disrupted in Alzheimer’s patients compared to healthy individuals, for example. How and where the cell makes BMP, however, had been unknown for decades.
After years of studying the protein encoded by CLN5 without discovering its function, Medoh wondered whether this might actually be BMP synthase, the long searched-for protein that makes BMP. “I’m not the first person to study CLN5 nor BMP, but I think I may be the first person who happened to study both at the same time, which is what allowed me to make this connection,” he said.
Medoh conducted a deceptively simple test: he mixed the molecular precursor to BMP with his mystery protein in a test tube. To see if the protein could transform the precursor into BMP, he used an instrument known as a mass spectrometer, which can detect the exact weights of individual molecules in a mixture. The resulting numbers are like a fingerprint that tell the researcher exactly what is in the sample. So, when Medoh mixed the precursor and the protein together, he was waiting to see a single number on the computer screen: 773, the mass of a molecule of BMP.
“When 773 appeared, I was the only person in the world who at that moment knew that this protein was the elusive BMP synthase. It was an intense dopamine rush,” said Medoh. “That really validated for me why I chose to pursue a PhD, and that is to make a discovery and be at the forefront of human knowledge.”
Cell rescue
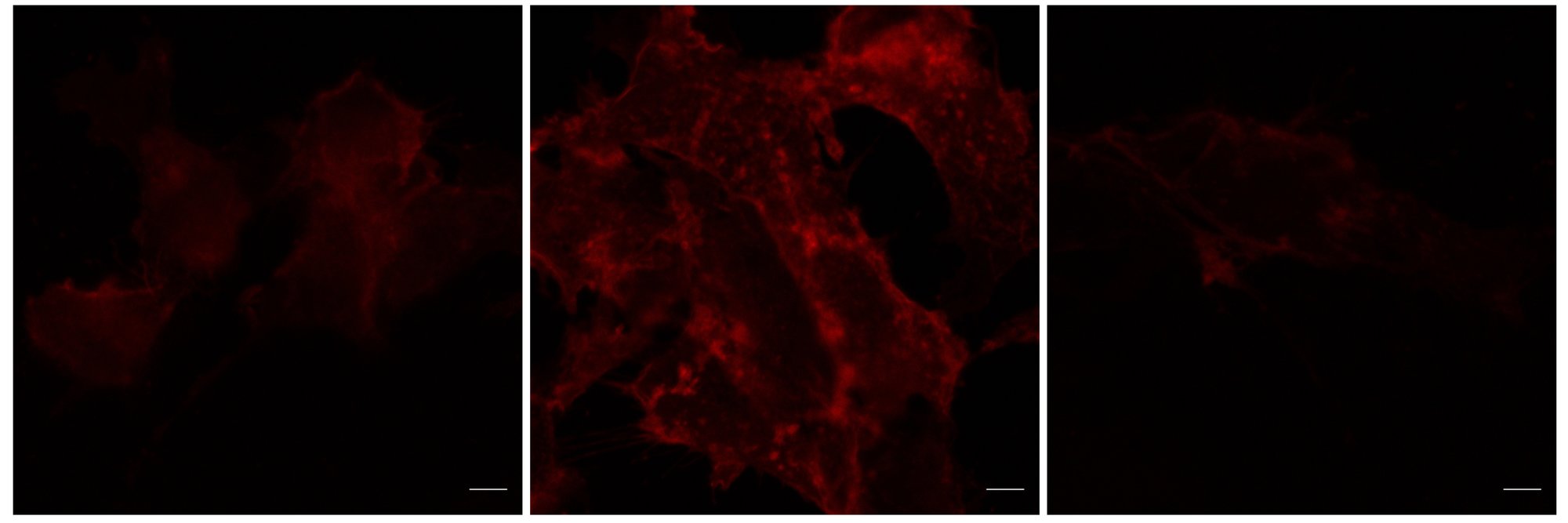
Abu-Remaileh needed more convincing evidence than a reaction in a test tube, devoid of the rest of the complex biochemistry happening in a cell. ”We now have to prove that this is relevant physiologically,” he said.
Medoh, who is also a fellow through the Sarafan ChEM-H Chemistry/Biology Interface (CBI) Training Program, used a diverse toolset with techniques borrowed from cell biology, genetics, and biochemistry to prove definitively that his mystery protein was in fact the BMP synthase.
For Abu-Remaileh, the key was a “rescue” experiment in cells. In this study, the team used cells with a CLN5 mutation, and collected and analyzed the lysosomes by mass spectrometry in collaboration with the Metabolomics Knowledge Center at Sarafan ChEM-H. They saw a decrease in BMP levels and corresponding increase in those of the precursor to BMP.
The researchers then “rescued” the cells by giving them CLN5 without the mutation. Normal BMP levels returned, and the team was convinced: the protein made by the CLN5 gene is the BMP synthase.
“BMP is important in major pathways that keep the lysosome functional and therefore keep individuals healthy, so it makes sense that this genetic mutation is exceedingly rare—its role is essential,” said Abu-Remaileh. “This approach shows that by studying these rare diseases, we can learn so much about fundamental biology and health.”
Now that scientists have identified the protein that creates BMP, they can potentially develop new kinds of medicine that will boost the protein’s activity and increase BMP levels, which could help both rare and common neurodegenerative diseases. Supported by the Knight Initiative for Brain Resilience and the Stanford Innovative Medicines Accelerator (IMA), the team is now doing just that.
Reimagining the lysosome
BMP was first discovered over 50 years ago, and since the 1970s, scientists have known that it is made in the cell and used in lysosomes. Though scientists have suspected it to be true, this is the first definitive proof that BMP is made inside the lysosome. This is also the first ever example of a lysosomal protein responsible for anabolism, or building a molecule, rather than catabolism, or degrading a molecule.
“For many people, lysosomal catabolism is synonymous with its function. Now we need to think about lysosomal anabolism, which expands how we think about lysosomal function,” said Medoh.
Other Stanford co-authors on the study include Andy Hims, a postbaccalaureate scholar in the Sarafan ChEM-H/Stanford Innovative Medicines Accelerator Postbaccalaureate Program in Target Discovery; Julie Chen; Ali Ghoochani; Kwamina Nyame; and Wentao Dong. Medoh is an O’Leary-Thiry Fellow and Nyame is a Kolluri Fellow, both through the Sarafan ChEM-H Chemistry/Biology Interface Training Program. Nyame is also the Mark and Mary Stevens Interdisciplinary Graduate Fellow at the Wu Tsai Neurosciences Institute. Abu-Remaileh is a Stanford-Terman Fellow and a Pew-Steward Scholar for Cancer Research.